COVID-19 Pandemic Accelerates Digitalization of Clinical Trials
Greenleaf Regulatory Landscape Series
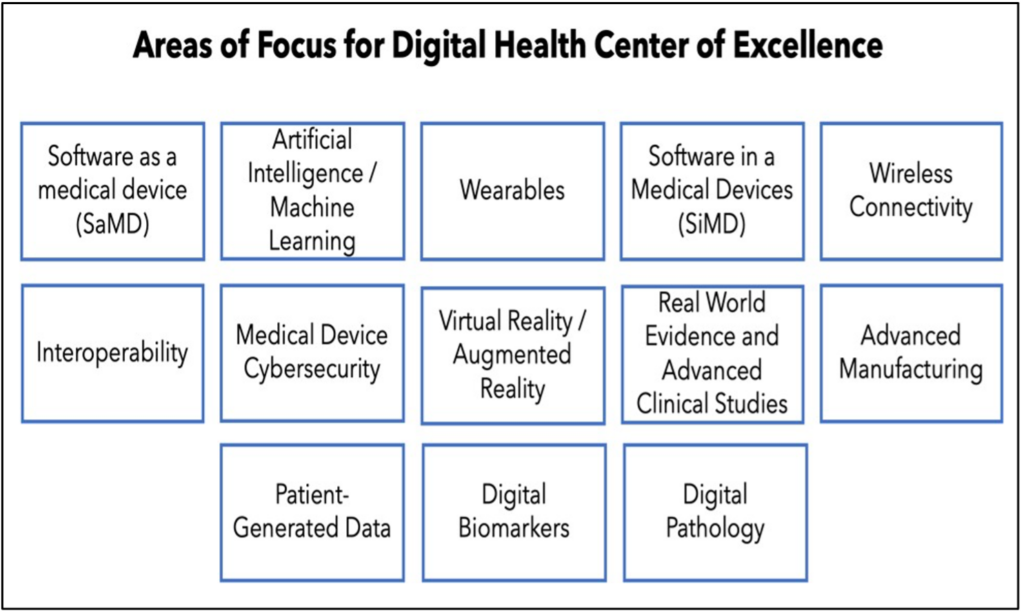
Recently the Food and Drug Administration (FDA or the Agency), led primarily by the Center for Devices and Radiological Health (CDRH), has been supporting multiple initiatives to promote the development of digital health technologies and to encourage the use of digital health tools (DHTs) in medical product development. In 2017, for example, the FDA published the Digital Health Innovation Action Plan, in which the FDA committed to hiring digital health experts and provided a timeline for issuing new digital health-focused guidances. This was followed by the launch of the Digital Health Center of Excellence (DHCOE) in August 2020. Sitting within CDRH, the DHCOE is intended to serve as a “one-stop shop” for all digital health-related inquires and will coordinate digital health activities both across the Agency and with other regulators internationally.
https://www.fda.gov/media/143078/download.
In the face of the COVID-19 pandemic, as the clinical trial enterprise seeks to maintain continuity while ensuring the safety of trial participants, the FDA’s digital health initiatives seem particularly well-timed. Indeed, during the past few months the use of DHTs have been critical in ensuring the continuity of disrupted trials by supporting remote data collection. During the pandemic, DHTs have been used to facilitate enrollment screening, conduct real-time safety monitoring, evaluate dose effects, and conduct endpoint assessments. In a recent survey of 245 clinical trial investigators, participants reported that 57% of patient interactions during ongoing trials were now conducted remotely.1 The same survey found that 77% of investigators expected the use of DHTs for remote patient monitoring to increase, while 54% expected an increase in use of DHTs to conduct electronic clinical outcomes assessments (eCOAs) and electronic patient reported outcome assessments (ePROs).2 This represents a marked increase over past DHT usage in medical product development, with DHTs only being used in 13% of registrational trials for the time period 2000 to 2018, according to recent research.3
A Regulatory Framework for DHTs
Acknowledging this trend, the FDA has requested funding in the PDUFA VII negotiations to support the development of a DHT framework to strengthen review capabilities of DHT- generated data in submissions, build staff capacity in digital health, and develop IT capacities to store and use DHT data.4 The FDA also shared in the summary report on the COVID-19 Pandemic Recovery and Preparedness Plan (PREPP) Initiative5 that that Agency is currently developing a guidance, which will be released this year, on the use of DHTs to capture study- related data directly from patients.
In the short term, the FDA has addressed the use of DHTs in the guidance “Conduct of Clinical Trials During the COVID-19 Public Health Emergency,”6 providing sponsors with recommendations on how to shift from in-person to remote assessments during the pandemic. In the guidance, the FDA provides sponsors with the flexibility to change the method of administration of clinical outcome assessments (COAs), specifically identifying performance outcomes (PerfO) assessments, interview-based clinician-reported outcome (ClinRO) assessments, PRO assessments, and observer-reported outcome (ObsRO) assessments as COAs that can be conducted remotely. In considering this change in administration, the FDA states that the change must be documented, and any additional variables related to the change should be included in the clinical trial data. The Agency also emphasizes the importance of prioritizing trial participant safety and privacy, maintaining data quality and integrity, and ensuring that both trial personnel and participants are appropriately trained on using any new technologies that are introduced.
DHTs in Clinical Trials
The emerging regulatory framework for DHTs in clinical trials is being built upon a regulatory paradigm that is already, in many respects, supportive of the remote collection of data in trials. As early as September 2013, the Agency addressed the use of DHTs to capture trial data in the guidance “Electronic Source Data in Clinical Investigations.”7 In the guidance, the FDA encourages electronic data capture, noting that it eliminates unnecessary duplication of data, reduces the possibility for transcription errors, and promotes real-time access for data review.
Although the FDA has not issued guidance specifically addressing the use of DHTs in clinical trials since 2013, the Agency has signaled an openness to the use of DHTs so long as they are fit for purpose, private and secure, and compliant with 21 CFR part 11.8 In public meetings and through work with the Clinical Trials Transformation Initiative (CTTI), the FDA has discussed how sponsors could best use digital technology to evaluate clinical benefit in trial participants. For example, prior to selecting a DHT, the FDA states that the concept being measured must be clinically meaningful, measuring what patients would like to see improved through treatment.9 Similarly, in selecting a technology, the sponsor should assess the reliability of the DHT through verification in the laboratory and validation in the field. On a practical level, sponsors also need to consider the technical aptitude and willingness to use a DHT among the population they are studying.10 As DHTs generate large volumes of data, sponsors should pre-specify how the data will be analyzed according to the data characteristics (e.g., intensity, frequency, event, etc.).11 Lastly, as previously noted, DHTs and DHT-generated data must be secure and participants’ privacy must be protected.
1. Xue, et al., “Clinical trial recovery from COVID-19 disruption,” Nature Reviews Drug Discovery, 10 Sept 2020, https://www.nature.com/articles/d41573-020-00150-9.
2. Ibid.
3. Mara, et al., “Quantifying the Use of Connected Digital Products in Clinical Research,” npj Digital Medicine 3, 50 (2020), https://www.nature.com/articles/s41746-020-0259-x.
4. U.S. Food and Drug Administration, “Prescription Drug User Fee Act (PDUFA) Reauthorization: FDA and Industry Digital Health and Informatics,” 30 Sept. 2020, https://www.fda.gov/media/143237/download.
5. FDA, “FDA COVID-19 Pandemic Recovery and Preparedness Plan (PREPP) Initiative: Summary Report,” January 2021, https://www.fda.gov/media/145129/download.
6. FDA, Guidance for Industry, “Conduct of Clinical Trials of Medical Products During the COVID-19 Public Health Emergency,” March 2020, https://www.fda.gov/media/136238/download.
7. FDA, Guidance for Industry, “Electronic Source Data in Clinical Investigations,” September 2013, https://www.fda.gov/media/85183/download.
8. 21 CFR part 11 establishes the criteria under which electronic records and electronic signatures are considered by the FDA to be trustworthy, reliable, and generally equivalent to paper records and handwritten signatures.
9. FDA, Draft Guidance for Industry, “Patient-Focused Drug Development: Methods to Identify What is Important to Patient,” October 2019, https://www.fda.gov/media/131230/download.
10. John Concato, Comments at FDA/CMS Summit, December 7, 2020.
11. Dashielle-Aje, Ebony, et al., ” Digital Health Technology Tools: Use in Clinical Investigations to Evaluate Clinical Benefit in Patients,” DIA Global Forum, June 2019, https://globalforum.diaglobal.org/ issue/june-2019/regulatory-perspective-digital-health-technology-tools/.